Prevention is the best weapon to win cancer. And it is within our reach, every day starting from the table, following the rules of proper nutrition, to finish the periodic medical checks. The concept of cancer prevention has begun to be emphasized, above all because, in recent decades, the incidence of this disease has increased. Everone should know the prevention of breast cancer. The reasons for growth are linked to the extension of the average life and a significant change in lifestyles. The increase in lung cancer cases in women, for example, is a direct consequence of the increase in the number of female smokers. Cigarette smoking, feeding and other causes such as viruses, hormones, and radiation appear among the factors identified in this study. Today the approach is multifactorial, ie the real risk for an individual to contract the disease is given by the combination of the different risk factors. Furthermore, it was understood that prevention measures are not limited only to the phases preceding the onset of the disease, but they can also be applied when the disease is already present.
Prevention of breast cancer
Primary prevention

There are two types of risk factors for the onset of cancer: those that can not be modified, such as sex, a particular genetic pattern and age, and those that can be modified, linked for example to lifestyle choices. The aim of primary prevention is to reduce the incidence of cancer by keeping modifiable risk factors under control and increasing individual resistance to these factors. In other words, it is a question of reducing the likelihood of a tumor appearing. A correct primary prevention strategy is not only based on the identification of risk factors but also and above all on the assessment of how the entire population or individual is exposed to these factors.
Prevention advice can be directed to the entire population or to particular categories of people considered. The primary prevention tools also include vaccines against specific infectious agents that increase the risk of cancer, such as the hepatitis B virus (liver tumor) or the Human Papilloma virus. The primary prevention strategies can be directed to the whole population or to particular categories of people considered. The primary prevention tools also include vaccines against specific infectious agents that increase the risk of cancer, such as the hepatitis B virus or the human Papilloma virus.
Secondary prevention
The aim of secondary prevention is to identify the tumor at a very early stage so that it can be treated effectively and consequently achieve a larger number of healings and a reduction in the mortality rate. Secondary prevention, therefore, coincides with early detection measures. Usually, it concerns the period between the biological onset of the disease and the manifestation of the first symptoms. For some types of cancer there are also national secondary prevention programs in Italy as in the case of mammography: the national screening Observatory, dependent on the Ministry, suggests a mammogram every two years for women aged 50 and over, but the cadence can vary depending on the doctor’s considerations on the personal history of each woman.
As for the Pap test, the Ministry of Health states that women from the beginning of active sexual life and, in any case, not more than 25 years should take the test every two to three years up to about 70 years of age, and offers the possibility to do it for free at the consultors. Prevention of breast cancer. The Regions are however autonomous in deciding if and how to propose such screening: in some cases, for example, the Pap test is free even at a young age, because the international indications are to start it from the age of first sexual intercourse. Many regions have also started colorectal screening campaigns, targeting the population between 50 and 70 years. In 1968 the World Health Organization (WHO) established the universal criteria according to which a disease affecting a large part of the population is suitable to be screened in advance:
With this type of screening, however, it is easier to identify tumors with a preclinical phase longer than those with rapid growth, especially when the average times between exam and the other are moderately long. This means that the cancer cases highlighted by the screening are also those that, by their very nature, have a more favorable prognosis. Finally, it should be noted that some cancers identified through secondary prevention screening do not give rise to a real disease, because in some cases the progression is very slow or even stops. It is not easy, however, to find out in which cases this happens and therefore for which types of cancer it is useful to do a screening and for which, instead, it is better to avoid. Prevention of breast cancer. In fact, identifying a tumor means proceeding with sometimes invasive tests or even with surgical interventions and therapies which in turn have side effects. It is in the delicate balance between benefits for the community and for the individual and damage from excess care that moves the world of prevention.
Tertiary prevention of breast cancer
Tertiary prevention of breast cancer means the prevention of so-called relapses (or relapses) or of possible metastases after the disease has been treated with surgery, radiotherapy or chemotherapy. It also embraces the field of adjuvant therapy, which prolongs the time intervals without disease and increases survival in many types of cancer such as testicles, breast, colon and many others.
How to prevent?
The victims of cancer, according to data from the World Health Organization, are constantly growing, so that it is estimated that in 2030 will exceed 11 million and that, in general, cancer will be the main cause of all deaths. It is estimated, however, that about 20-30% of cancers can be prevented by adopting correct lifestyles (quit smoking, eating healthy and balanced) and subjecting themselves regularly to visits and screening exams.
What is a risk factor?

The risk factor is all that can affect or modulate the development of cancer. There are two different types of risk factors, ie those modifiable (behavior and environment) and those that can not be modified. The effects of these factors depend on many variables including duration and type of risk exposure or the combined effect of two or more factors.
How are risk factors identified?
There are various methodologies that allow us to classify a substance or behavior as a risk factor: we go from molecular experiments, which aim to identify a genetic alteration, to epidemiological studies that evaluate how the factors related to lifestyle or environment are related to the onset of particular tumors.
The interaction between genetic and environmental risk factors
On the basis of the most recent data, it is clear that in almost all tumors it is possible to identify an alteration of the DNA that plays a major role in the onset of the disease, but generally environmental factors cooperate with the genetic ones at the beginning and cancer propagation. Mathematical models have been created that establish the risk of cancer which based on the presence or absence of one or more risk factors and on the interaction between them. Specifically, the models define whether an individual is at high or low risk of cancer, but also specify that not necessarily a subject who has a high risk will develop the disease and at the same time do not rule out the possibility that those with a low risk may be hit by a tumor.
Prevention: why?
The ultimate goal of identifying and controlling risk factors is to reduce the risk and therefore mortality or at least the risk of developing cancer, but because the development of cancer often covers a very long time span (even tens of years) ), it is important to identify intermediate objectives (for example, precancerous lesions). Prevention of breast cancer. It should be noted, however, that these intermediate objectives have limits. For example, it is said that a precancerous lesion must turn into cancer or, conversely, that a negative result at a screening is equivalent to a zero risk.
The role of biomarkers
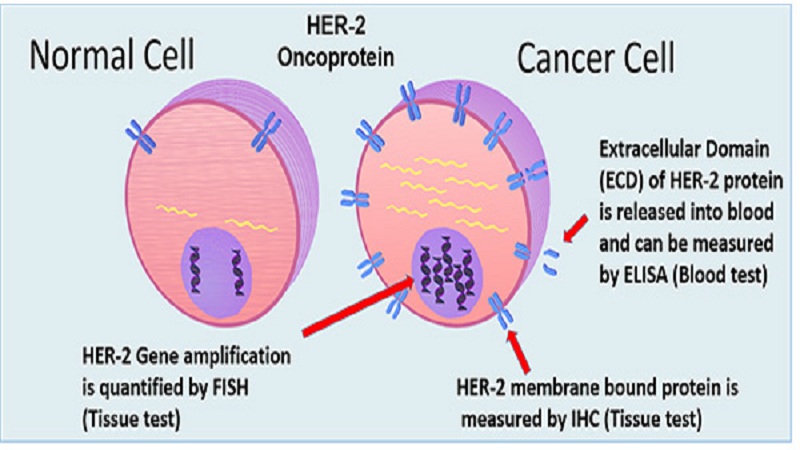
The so-called biomarkers, or simply markers, are part of the new tools to determine the risk of cancer: these are molecules that, if present or absent in the blood, allow to understand if a person is at risk of developing a certain type of tumor. In some cases, they also allow establishing the response to therapy or the progression of the disease. Among the best-known biomarkers, we can mention PSA (prostate specific antigen) for prostate cancer, which is present at high levels in prostate tumors (but also in benign prostate hypertrophy) and estrogen receptors for breast cancer, which provide useful indications in terms of prognosis and choice of therapy.
Conclusion
Cancer is a serious disease nowadays. Every one should aware of this. Everyone should know about the prevention of breast cancer. If you want some information this article must help you. Thank You.





